WE TAKE PAIN RELIEF SERIOUSLY. EVERYTHING ELSE? MEH.

GET THE STRONGEST ALL-NATURAL & ORGANIC TOPICAL PAIN CREAM ON THE MARKET TODAY...& THE MOST INTERESTING.

PUNCHING PAIN IN THE FACE SINCE 2011.

WANT TO BE A WHOLESALE PARTNER? CLICK HERE

WE TAKE PAIN RELIEF SERIOUSLY. EVERYTHING ELSE? MEH.

GET THE STRONGEST ALL-NATURAL & ORGANIC TOPICAL PAIN CREAM ON THE MARKET TODAY...& THE MOST INTERESTING.

PUNCHING PAIN IN THE FACE SINCE 2011.

WANT TO BE A WHOLESALE PARTNER? CLICK HERE

WE TAKE PAIN RELIEF SERIOUSLY. EVERYTHING ELSE? MEH.

GET THE STRONGEST ALL-NATURAL & ORGANIC TOPICAL PAIN CREAM ON THE MARKET TODAY...& THE MOST INTERESTING.

PUNCHING PAIN IN THE FACE SINCE 2011.

WANT TO BE A WHOLESALE PARTNER? CLICK HERE

WE TAKE PAIN RELIEF SERIOUSLY. EVERYTHING ELSE? MEH.

GET THE STRONGEST ALL-NATURAL & ORGANIC TOPICAL PAIN CREAM ON THE MARKET TODAY...& THE MOST INTERESTING.

PUNCHING PAIN IN THE FACE SINCE 2011.

WANT TO BE A WHOLESALE PARTNER? CLICK HERE

WE TAKE PAIN RELIEF SERIOUSLY. EVERYTHING ELSE? MEH.

GET THE STRONGEST ALL-NATURAL & ORGANIC TOPICAL PAIN CREAM ON THE MARKET TODAY...& THE MOST INTERESTING.

PUNCHING PAIN IN THE FACE SINCE 2011.

WANT TO BE A WHOLESALE PARTNER? CLICK HERE

WE TAKE PAIN RELIEF SERIOUSLY. EVERYTHING ELSE? MEH.

GET THE STRONGEST ALL-NATURAL & ORGANIC TOPICAL PAIN CREAM ON THE MARKET TODAY...& THE MOST INTERESTING.

PUNCHING PAIN IN THE FACE SINCE 2011.

WANT TO BE A WHOLESALE PARTNER? CLICK HERE

The Vagus Nerve: A Key Player in Chronic Pain Management
4 lire la lecture
Table of Contents

- Introduction
- Understanding the Vagus Nerve
- Chronic Pain: A Multifaceted Challenge
- The Vagus Nerve and Pain Modulation
- Vagus and the Inflammatory Reflex
- Psychological and Stress-Related Aspects
- Future of Vagus Nerve Research
- Conclusion
- References
Introduction

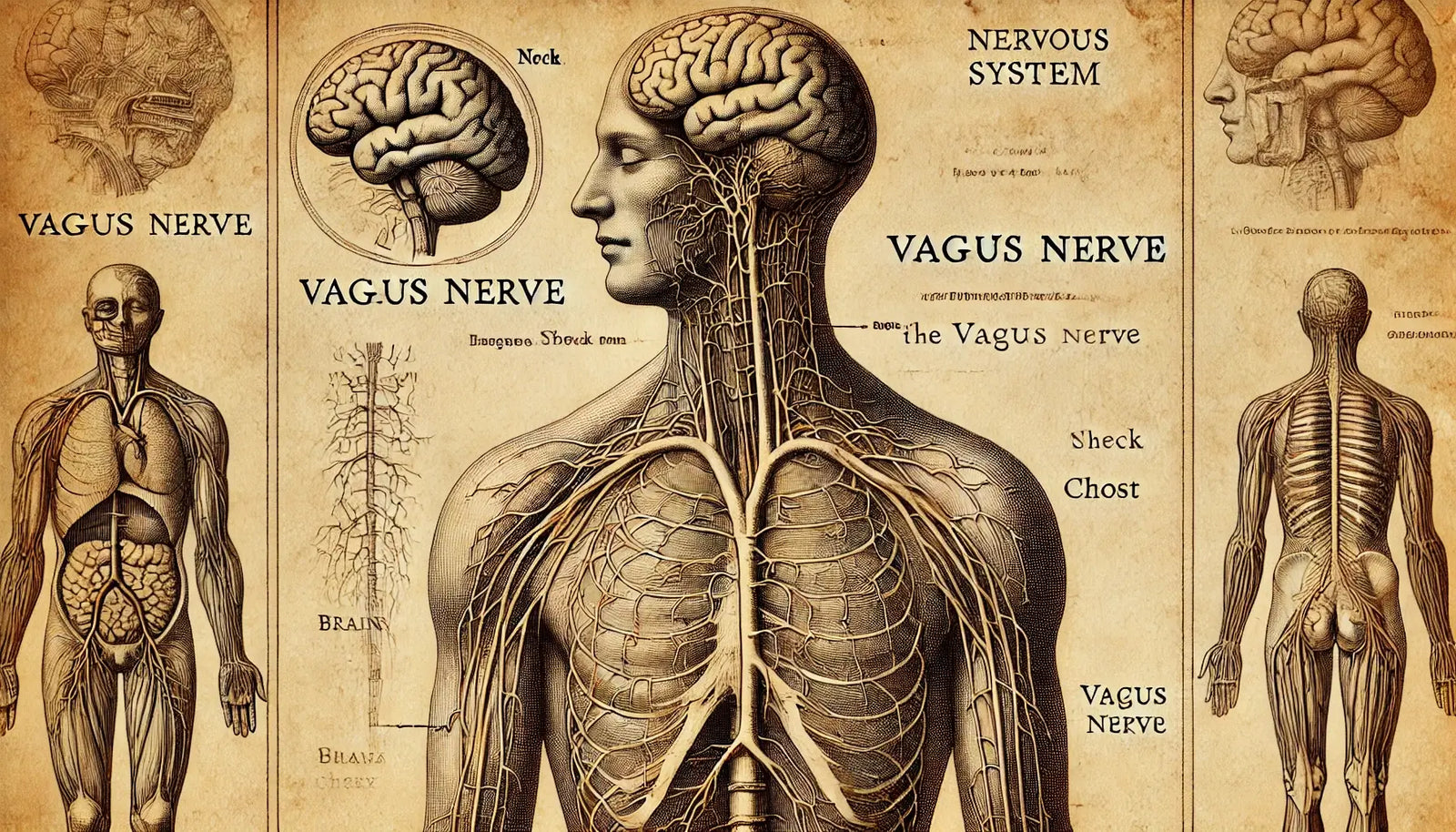
The vagus nerve, the tenth cranial nerve, is one of the longest and most complex nerves in the human body. It extends from the brainstem through the neck and thorax down to the abdomen, innervating various organs, including the heart, lungs, and digestive tract. Often referred to as the "wanderer" due to its extensive reach, the vagus nerve plays a crucial role in the autonomic nervous system, regulating functions like heart rate, digestion, and immune response. Recently, research has highlighted its strong analgesic effects(1) and significant link to chronic pain, offering new insights and potential therapeutic avenues.

Understanding the Vagus Nerve

The vagus nerve is primarily involved in parasympathetic nervous system activities, often described as "rest and digest" functions. It helps calm the body after stress by slowing the heart rate, enhancing digestion, and reducing inflammation. Its ability to modulate inflammation is particularly important, as chronic pain is frequently associated with persistent inflammatory states.
Chronic Pain: A Multifaceted Challenge

Chronic pain is a pervasive and debilitating condition affecting millions worldwide. Unlike acute pain, which serves as a warning signal of injury or disease, chronic pain persists for months or even years, often without a clear cause. It can result from various conditions, such as fibromyalgia, arthritis, neuropathy, and even prolonged stress. The complexity of chronic pain lies in its multifactorial nature, involving physical, psychological, and neurobiological components(2). In any of these cases, the nervous system is affected. The vagus nerve is only one component of this entire system, but studies are showing that it plays a much more important role than we previously realized.

The Vagus Nerve and Pain Modulation

Research has increasingly focused on the vagus nerve's role in pain modulation. Vagus nerve stimulation has been broken down into two categories: invasive and non-invasive. Both methods have been shown to modulate pain sensation, increase parasympathetic nervous system response, and systemic inflammatory response. The nerve's anti-inflammatory properties are central to this interest. It has been shown that the vagus nerve can inhibit the release of pro-inflammatory cytokines, thereby reducing inflammation and potentially alleviating pain.
Vagus Nerve Stimulation (VNS)
One of the most promising developments in this field is vagus nerve stimulation (VNS). VNS involves delivering electrical impulses to the vagus nerve via a small device implanted under the skin. Originally used to treat epilepsy and depression, VNS has shown potential in managing chronic pain conditions. Studies have demonstrated that VNS can reduce pain severity and improve the quality of life in patients with conditions like rheumatoid arthritis and fibromyalgia.
Non-Invasive VNS
In addition to implanted devices, non-invasive VNS techniques have emerged. These methods, which involve stimulating the vagus nerve through the skin of the neck or ear, offer a less intrusive alternative with fewer side effects. Preliminary research suggests that non-invasive VNS may be effective in reducing pain and improving mood in chronic pain patients. Since this method is accessible to many people, there continues to be strong interest in this safe, natural way to stimulate the vagus nerve.

The Inflammatory Reflex

The vagus nerve is a critical component of the body's "inflammatory reflex," a mechanism that controls immune response and inflammation. When activated, the vagus nerve sends signals that dampen the production of inflammatory molecules. This neural-immune interaction underscores the potential of targeting the vagus nerve to manage chronic inflammatory conditions that contribute to chronic pain.
Psychological and Stress-Related Aspects

Chronic pain is not merely a physical phenomenon; it is often intertwined with psychological factors such as stress, anxiety, and depression. The vagus nerve, through its parasympathetic functions, helps regulate stress responses and promote relaxation. Enhancing vagal tone, the activity level of the vagus nerve, has been associated with improved stress resilience and emotional regulation, which can indirectly alleviate pain by reducing stress-related exacerbations.
Future of Vagus Nerve Research

The link between the vagus nerve and chronic pain is an exciting frontier in pain management research. Future studies are needed to better understand the mechanisms by which vagal modulation affects pain perception and inflammation. Additionally, exploring personalized approaches to VNS, considering individual variations in vagus nerve anatomy and function, could optimize therapeutic outcomes.
Conclusion

The vagus nerve's extensive influence on the body's physiological and psychological processes positions it as a pivotal player in chronic pain management(3). From its anti-inflammatory capabilities to its role in stress regulation, the vagus nerve offers a multifaceted approach to tackling chronic pain. As research progresses, therapies targeting the vagus nerve, including both invasive and non-invasive VNS, hold promise for providing relief to the millions affected by chronic pain, improving their quality of life and paving the way for innovative pain management strategies.
References
1. Review of the Uses of Vagal Nerve Stimulation in Chronic Pain Management Chakravarthy K, Chaudhry H, Williams K, Christo PJ. Review of the Uses of Vagal Nerve Stimulation in Chronic Pain Management. Curr Pain Headache Rep. 2015 Dec;19(12):54. doi: 10.1007/s11916-015-0528-6. PMID: 26493698.
2. Comprehensive Evaluation for Chronic Pain Fidler SK. Comprehensive Evaluation for Chronic Pain. Prim Care. 2022 Sep;49(3):375-385. doi: 10.1016/j.pop.2022.02.001. Epub 2022 Aug 29. PMID: 36153080.
3. Role of Vagus Nerve Stimulation in the Treatment of Chronic Pain Shao P, Li H, Jiang J, Guan Y, Chen X, Wang Y. Role of Vagus Nerve Stimulation in the Treatment of Chronic Pain. Neuroimmunomodulation. 2023;30(1):167-183. doi: 10.1159/000531626. Epub 2023 Jun 27. PMID: 37369181; PMCID: PMC10614462.
Laisser un commentaire
Les commentaires sont approuvés avant leur publication.
Voir l'article entier

Why a Safe Space Is Essential for Pain Relief and Injury Healing in Athletes
6 lire la lecture
Every athlete wants to speed healing from injury and get back to sport safely. One of the most overlooked and underestimated parts of any recovery program is the safe space. Find out why creating a physical and psychological safe space for healing is the foundation to any injury rehabilitation & pain management plan.

Essai de capsaïcine pour la douleur au genou
1 lire la lecture
Les résultats actuels Les résultats de cette étude soutiennent l'efficacité et la sécurité de l'injection intra-articulaire de trans‐capsaïcine pour gérer la douleur modérée à sévère associée à l'arthrose du genou. Les résultats indiquent que des développements cliniques plus poussés sont justifiés.
Voir l'article entier

Douleur chronique : nouvelles recherches, nouveaux traitements
1 lire la lecture
Il y a à peine 20 ans, on disait trop souvent aux personnes souffrant de douleur chronique que leur problème était « dans leur tête » ou qu'elles étaient hypocondriaques. Mais au cours de la dernière décennie, une poignée de chercheurs dévoués ont appris que la douleur chronique n’est pas simplement le symptôme de quelque chose d’autre – comme l’anxiété , la dépression ou un besoin d’attention – mais une maladie à part entière.
Voir l'article entier
Heading
Text area can be used for details about blog authors or general information.
Subscribe
Sign up to get the latest on sales, new releases and more …

Signup for our Newsletter
Get current pain research, the latest discounts, inspiring stories, and much more delivered right to your inbox. Never spam, always top-notch information.